Knowledge is power when it comes to embarking on any medical procedure.


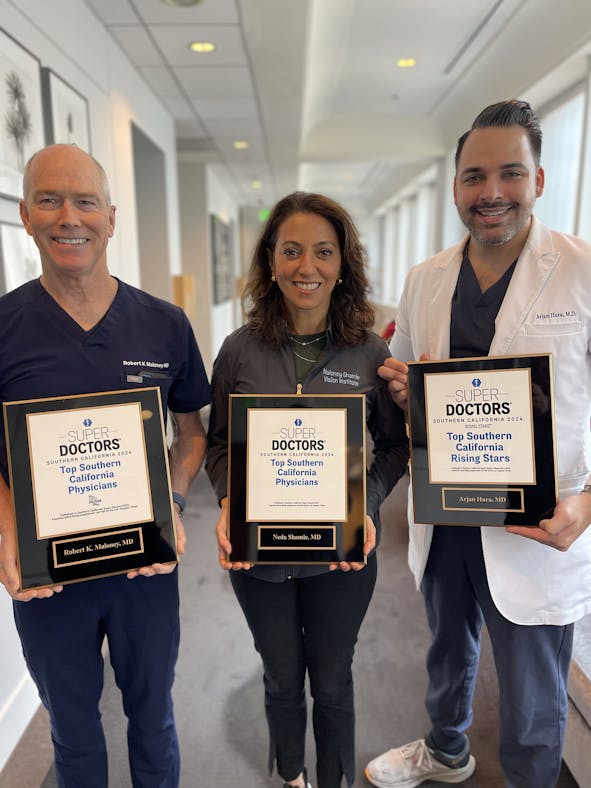
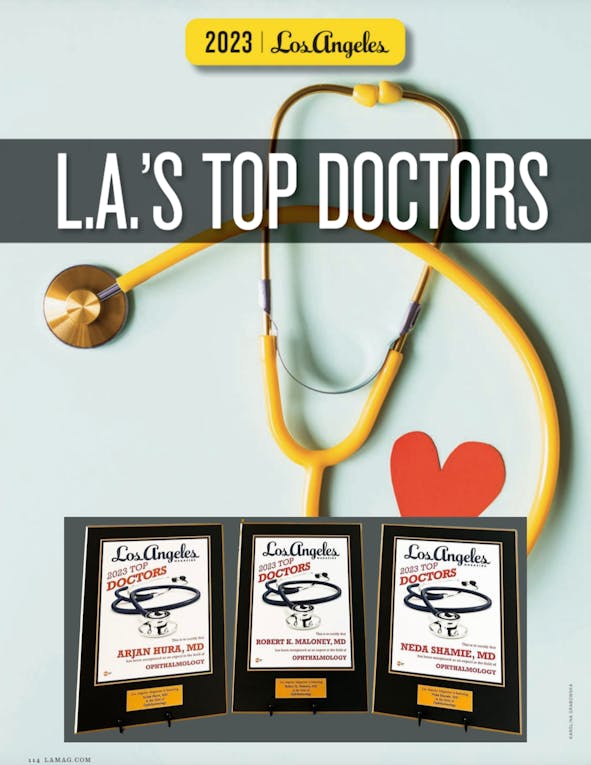
Our surgeons believe that a well-informed patient is key to successful vision correction surgery. They want to be sure that you fully understand what you can expect from the procedure you choose. Their goal is to help you care for and preserve your eyesight in the best way possible. Here, you can find the information that you need to help you make informed choices about health care for your eyes.
See Better Now
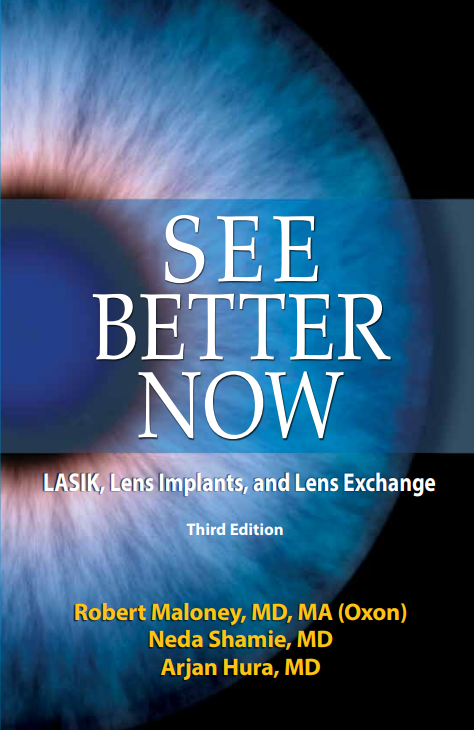
by Robert K. Maloney, MD, MA (OXON), Neda Shamie MD, Arjan Hura, MD - Addicus Books, Omaha, Nebraska
Cataract Surgery
by Robert K. Maloney, MD, MA (OXON), Neda Shamie MD, Arjan Hura, MD - Addicus Books, Omaha, Nebraska
Lasik: A Guide To Laser Vision Correction
by Robert K. Maloney, MD, MA (OXON), Neda Shamie MD, Arjan Hura, MD - Addicus Books, Omaha, Nebraska