TAKE-HOME MESSAGE
- Recognize that partial coherence interferometry is a reproducible measurement of axial length.
- Regularly update the IOL constants in your IOLMaster.
- Approach multifocal IOLs cautiously and consider using toric IOLs when appropriate.
No. 4: Approach multifocal IOLs cautiously. In the early days of laser refractive surgery, the small optical zone treatment often created a multifocal effect, and some patients were unhappy. As lasers became more monofocal, with larger optical zones and wavefront-guided treatments, patients were happier with the outcomes. In the future, improved accommodating IOLs should lessen the need for multifocals.
No. 5: Keep your eye on new technologies. We may soon have IOLs that can be adjusted noninvasively after they are in the eye, such as the Light Adjustable Lens (LAL; Calhoun Vision, Inc., Pasadena, CA). It is made from a photosensitive polymer that responds to UV light postoperatively by changing shape. In clinical trials, the LAL allowed the correction of up to 2.00 D of myopia, hyperopia, and astigmatism.8-10 The LAL may also allow control of spherical aberration, providing an expanded depth of near focus (personal communication, Pablo Artal, MD, PhD, May 2009). The LAL is available commercially in Europe and is currently in FDA phase 2 trials. When that time comes, we will confidently be able to say that cataract surgery is indeed a modern refractive procedure.
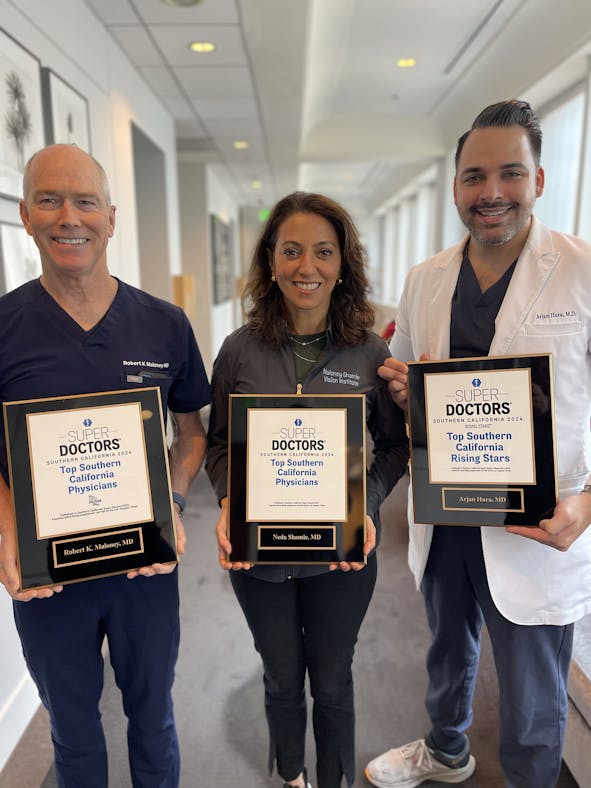
Robert K. Maloney, MD, is in private practice and is one of the Directors of the Maloney-Shamie-Hura Vision Institute in Los Angeles. He is the chief medical officer of Calhoun Vision, Inc., and a consultant to Abbott Medical Optics Inc. Dr. Maloney may be reached at 877-999-3937; [email protected].
- Waring GO III, Casebeer JC, Dru RM. One-year results of a prospective multicenter study of the Casebeer system of refractive keratotomy. Casebeer Chiron Study Group. Ophthalmology. 1996;103(9):1337-1347.
- Slade SG, Durrie DS, Binder PS. A prospective, contralateral eye study comparing thin-flap LASIK (sub- Bowman Keratomileusis) with photorefractive keratectomy. Ophthalmology. 2009;116(6):1075-1082.
- Summary of Safety and Effectiveness Data. US FDA Web site. http://www.fda.gov/ohrms/dockets/dockets/05m0117/05m-0117-aav0001-03-SSED-vol1.pdf. Accessed August 28, 2009
- Randleman JB, Foster JB, Loupe DN, et al. Intraocular lens power calculations after refractive surgery: consensus-K technique. J Cataract Refract Surg. 2007;33(11):1892-1898.
- Leccisotti A. Intraocular lens calculation by intraoperative autorefraction in myopic eyes. Graefes Arch Clin Exp Ophthalmol. 2008;246(5):729-733.
- Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85:472-485.
- Mendicute J, Irigoyen C, Ruiz M, et al. Toric intraocular lens vs. opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg. 2009;35:451-458.
- Hengerer FH, Mellein AC, Buchner SE, Dick HB. The light-adjustable lens. Principles and clinical applications. Ophthalmology. 2009;106(3):260-264.
- Chayet A, Sandstedt CA, Chang SH, et al. Correction of myopia after cataract surgery with a lightadjustable lens [published online ahead of print November 20, 2008]. Ophthalmology. 2009.
- Chayet A, Sandstedt CA, Chang SH, et al. Correction of residual hyperopia after cataract surgery using the light-adjustable intraocular lens technology. Am J Ophthalmol. 2009;147(3):392-397.