GLOSSARY
20/20 vision: Normal visual acuity. The numbers indicate that the tested eye, twenty feet away from the eye chart, sees as well as a "normal" eye at the same distance.
Ablation: Removal, or vaporization, of tissue with a laser.
Accommodating intraocular lens: A type of intraocular lens (IOL) that enables the patient to focus automatically, via "retraining" of the ciliary muscle and zonules, at a range of distances in much the same way as with a clear, flexible natural lens.
Accommodation: The eye's ability to change lens shape (by action of the ciliary muscle and zonules) in order to focus clearly on objects at various distances. As the lens becomes more rigid with age-a condition called presbyopia-it is less able to accommodate.
Adaptive intraocular lens: See accommodating intraocular lens.
Aftercataract: Opacity that develops on the posterior lens capsule after extracapsular cataract removal.
Amblyopia: Poor vision, usually in one eye but occasionally in both eyes, that develops between birth and age six. Caused by continued suppression of vision in the affected eye, not by structural abnormality.
Amsler grid: Grid consisting of lines on contrasting background (black on white or white on black) used to test for macular degeneration or other central-visual-field defects.
Anterior chamber: Area between the cornea and the iris filled with aqueous humor.
Antioxidant: Molecule or compound, such as vitamins C and E and selenium, that can bond with and neutralize free radicals, preventing cell damage.
Aphakia: Absence of the crystalline lens of the eye.
Aqueous, aqueous humor: Clear, watery fluid that fills the anterior chamber of the eye; maintains intraocular pressure and nourishes the cornea, iris, and lens.
A-scan: Ultrasound device used to distinguish normal from abnormal eye tissue or to measure eye length.
Aspheric intraocular lens: A type of IOL that is slightly flattened around the edges; believed to offer better contrast sensitivity than traditional IOLs, on which the front surface is curved.
Astigmatism: Visual distortion caused by a cornea whose surface is elongated-like the side of a football-rather than curved like an arc on a sphere. Light rays enter the eye unequally and may produce two focal points on the retina.
Astigmatism management: A surgical procedure designed to prevent or minimize worsening of astigmatism, a common side effect of cataract surgery.
Autorefractor: A device, used to test refractive error, that emits a pinpoint beam of light, which reflects off the retina and measures the eye's response.
Best corrected visual acuity (BCVA): The best vision possible with corrective lenses.
Bioavailability: The ease with which a nutrient is absorbed and used by the body.
Biological age: A person's age measured by the condition of the muscles, brain, lungs, and sensory organs, unlike chronological age, measured in calendar years.
Biomicroscope: See slit lamp.
Blind spot: Sightless area within normal visual field; caused by absence or blockage of light-sensitive photoreceptors on the retina (specifically the fovea).
Blue-blocking intraocular lens: An IOL that filters out high-energy blue light, which can damage the retina and contribute to macular degeneration.
Blunt cannula: A narrow tube with a blunted tip, designed to perform many of the piercing functions of a surgical needle but without the needle stick.
Brunescence: Browning of the crystalline lens due to cataracts.
Capsule: A thin membrane that forms the outermost layer of the crystalline lens, above the cortex and the nucleus.
Cataract: Clouded area (opacity) of the crystalline lens; caused by trauma, disease, or aging, or may be congenital.
Central vision: In the visual field, the area of sharpest vision, used for reading and distinguishing detail and color. See also peripheral vision.
Choroid: Layer of blood vessels that provide oxygen and nutrients to the retina.
Ciliary body: Eye structure that contains ciliary muscle, which contracts or relaxes, thereby changing the shape of the crystalline lens and allowing it to focus on objects at varying distances.
Ciliary muscle: See ciliary body.
Clear-corneal phacoemulsification: An advanced type of cataract surgery in which the incision is placed at the edge of the clear cornea. Clear-corneal phacoemulsification does not require the use of needles, does not cause bleeding, uses a very small (one-eighth of an inch or smaller) incision, and allows for rapid recovery.
Color blindness: Inability to clearly distinguish certain colors. So-called red-green color blindness is usually hereditary. Yellowing of cataracts can also cause a degree of color blindness.
Cone: One of more than 7 million retinal photoreceptor cells (in each eye) concentrated in the macular area (specifically the fovea centralis) of the retina, responsible for sharp vision and ability to see colors.
Congenital cataract: A cataract that is present at birth.
Conjunctiva: Clear mucous membrane that covers the white of the eye (sclera) and lines the inner surface of the eyelids.
Contrast sensitivity: Ability to visually distinguish dark objects against a light-colored background, or light-colored objects against a dark background.
Cornea: Clear, curved protrusion at the front of the eye through which light first passes; provides 70 percent of the eye's focusing power. The cornea covers and protects the iris, pupil, and anterior chamber.
Corneal edema: Abnormal fluid buildup and consequent swelling of the cornea.
Corneal pachymetry: Measurement of corneal thickness using ultrasound.
Corneal topography: Rendering of a precise three-dimensional map of the cornea using sophisticated camera and computer technology.
Cortex: Soft, clear tissue that forms the middle layer of the crystalline lens, between the capsule and the nucleus.
Cortical cataract: A cataract that begins as whitish, wedge-shaped opaque areas on the outer edge of the lens cortex, near the capsule, eventually becoming streaks reaching inward to the center of the lens, like spokes on a wheel.
Cosmic radiation: Atomic radiation that bombards Earth from outer space. Earth's atmosphere provides protection from these harmful rays, which can cause cataracts in airline pilots and astronauts.
Cover test: Part of an eye examination, often used to detect strabismus or amblyopia. While the patient looks directly at an object, the eye doctor covers one eye and quickly notes how much the uncovered eye moves to adjust.
Cross-eye: See esotropia.
Crystalline lens: The eye's natural lens; a flexible, transparent tissue, located behind the iris, that helps focus rays of light onto the retina.
Cystoid macular edema: A condition in which fluid-filled cysts develop in the macula, causing retinal swelling.
Diabetes mellitus: A group of diseases that develop when the body is unable to use blood sugar for energy, causing excessive amounts of sugar in the bloodstream (hyperglycemia).
Dilation: Enlargement (of an opening). With reference to the eye, dilation of the pupil occurs naturally in dim light, allowing more of the available light into the eye. Eye doctors also chemically dilate the pupil during an eye examination in order to have a better view into the interior of the eye.
Diopter: A measurement of refractive error-a positive number in the case of hyperopia (farsightedness), and a negative number to describe myopia (nearsightedness).
Diplopia: See double vision.
Double vision: A type of distortion in which two images of a single object are seen. Common with cataracts and other eye disorders.
Emmetropes: People who have no refractive error; that is, no nearsightedness, farsightedness, or astigmatism. Perfect refractive ability is referred to as emmetropia.
Endophthalmitis: A serious infection, usually bacterial, of the interior of the eye.
Epithelium: The cornea's outermost layer of cells, forming the eye's first defense against infection.
Esotropia: Lack of coordination between eye movements in which one eye is normally aligned and the other is aligned inward. Also called "cross-eye." See also strabismus.
Excimer laser: A "cold" laser, so called because it can remove corneal tissue without heating it during refractive surgery.
Exotropia: Lack of coordination between eye movements in which one eye is normally aligned and the other is aligned outward. Also called "wall-eyes."
Extracapsular cataract surgery: A form of cataract surgery, such as phacoemulsification, that leaves much of the lens capsule in place to support the new lens and help with healing. The term also refers to the more-invasive extracapsular procedure that was common before phacoemulsification, involving a larger incision, removal of the intact nucleus, approximately ten sutures, and an extended recovery period.
Eyelid: Thin, retractable tissue covering the front of the eye. The eyelid serves to protect the eye from dust and other foreign objects and from exceedingly bright light. It also distributes moisture (tears) over the cornea.
Farsightedness: See hyperopia.
Field of vision: See visual field.
Floaters: Particles in the vitreous humor that drift across the visual field.
Folding intraocular lens: An IOL that can be inserted through a tiny incision by being folded or rolled; it then opens to normal size within the eye.
Fovea, fovea centralis: Central concave area of the macula that is packed with photoreceptors called cones, which produce the sharpest vision.
Free electron: The unpaired electron in a free radical.
Free radical: An atom, usually oxygen, that has an odd number of electrons, leaving one electron unpaired and making the atom unstable.
Fundus: Interior surface of the back of the eyeball, visible with an ophthalmoscope. The eye's fundus includes the retina (with macula and fovea) and the juncture of the optic nerve with the eye.
Ghost images: Distortion of vision similar to "seeing double." With double vision, however, you'll see two relatively clear images, whereas ghost images are fainter "copies" that appear on one side of or around the object you're looking at.
Ghosting: A type of image distortion, fairly common with cataracts. See also ghost images.
Glare: Sensation of dazzling, intense, scattered light when looking at light source; often due to cataracts.
Glassblower's cataract: A cataract that is caused by infrared (heat) radiation, usually as a result of occupational exposure, as in the case of arc welders and glassblowers.
Glaucoma: Group of diseases usually associated with increased intraocular pressure; if untreated, can lead to blindness.
Gonioscope: Device used to examine the eye's anterior chamber, using a magnifier and mirror-equipped contact lens.
Halo: Perceived rings around light sources viewed at night; often accompanied by glare. A common symptom of cataracts.
Haptics: The side struts, or extensions, on an intraocular lens that help to hold it in place after implantation.
Hypermature cataract: A cataract that is so far advanced it may be completely opaque and allow little or no vision in the affected eye; can cause pain and inflammation.
Hyperopia: Farsightedness, occurring when the eye is "too short" and images come into focus behind the retina. A farsighted person, or hyperope, may see well at a distance but have trouble with near vision.
Immature cataract: A cataract that is not well advanced, cannot be seen with the naked eye, and may not yet interfere significantly with vision.
Intracapsular cataract surgery: A type of cataract surgery, rarely used today, that involves removal of the entire lens, including the capsule.
Intraocular lens: A synthetic lens implanted during cataract surgery to replace the natural lens.
Intraocular pressure (IOP): Fluid pressure within the eye.
IOL: See intraocular lens.
Iris: The colored ring in the visible eye. Contracts or recedes around the pupil to regulate the amount of light that enters the eye.
Keratotomy: A surgical incision of the cornea.
Laser: Acronym for light amplification by stimulated emission of radiation, a high-energy light source used medically to cut, burn, or dissolve tissues.
LASIK: Acronym for laser assisted in situ keratomileusis, a refractive-surgical procedure to reshape the cornea and change its optical power.
Lazy eye: See amblyopia.
Legal blindness: Best corrected visual acuity of 20/200 or worse.
Lens: See crystalline lens.
Limbal-relaxing incisions: An astigmatism-management technique consisting of small incisions in the limbus-the thin connection between the cornea and the white of the eye (the sclera)-that cause the cornea to become more rounded when it heals.
Low vision: Poor visual acuity.
Macula: Small central area of the retina filled with light-sensitive photoreceptors called rods and cones.
Macular degeneration: A progressive eye disease caused by deterioration of the central portion of the retina, called the macula.
Mature cataract: A cataract that has advanced to the point where the lens appears milky.
Monofocal intraocular lens: An IOL that is similar to a disposable camera lens, in that it has a single fixed focal point, usually designed for mid-distance vision. Eyeglasses are needed for good vision at other distances.
Monovision: Adjustment, using corrective lenses or surgery, of one eye for near vision and the other for distance vision.
Multifocal intraocular lens: An IOL that is similar to a sophisticated camera lens, in that it automatically adjusts its focus to provide good near, mid-range, and distance vision without glasses.
Myopia: Nearsightedness, occurring when the eye is "too long" and images come into focus before they reach the retina. A nearsighted person, or myope, may have good near vision but have difficulty seeing objects at a distance.
Nearsightedness: See myopia.
Noncontact tonometry: A method of measuring intraocular pressure (that is, pressure of fluids within the eye) in which the testing instrument does not come in contact with the cornea.
Nuclear cataract: Clouding of the center of the lens (nucleus), almost always due to aging.
Nucleus: The firm center, or core, of the crystalline lens, surrounded by the cortex, which in turn is inside the capsule.
Ophthalmologist: A medical doctor who specializes in the diagnosis and medical or surgical treatment of eye disorders and disease.
Ophthalmoscope: An illuminated instrument using mirrors to examine structures in the back of the eye.
Optic nerve: Bundle of nerve fibers that transmit visual impulses from the retina to the brain.
Optical coherence biometry: Measurement of eye length using light, rather than ultrasound as in an A-scan.
Optician: One who is trained to fit and dispense eyeglasses and, in some U.S. states, contact lenses, according to a prescription from an optometrist or ophthalmologist. Outside the United States, some countries license ophthalmic opticians to do eye exams.
Optometrist: A doctor of optometry (O.D.), qualified to diagnose and treat vision disorders not requiring specialized medical or surgical intervention.
Orbit: The bony socket that surrounds the eyeball.
Overripe cataract: See hypermature cataract.
Pachymetry: Measurement of corneal thickness.
Perimeter: A device that emits flashes of light to test field of vision and reveal blind spots.
Peripheral vision: Side vision; in the visual field, perception of objects outside the direct line of vision. See also central vision.
Phacoemulsification: Surgical procedure to remove a cataract using ultrasound to break up the lens, which is then removed by suction.
Phoropter: An eye-examination device consisting of a complete range of corrective lenses that can be adjusted to hundreds of combinations, which the patient is asked to evaluate. By continually changing the lenses, the doctor can arrive at a combination of lens strengths that becomes the basis of a prescription for corrective lenses.
Photoreceptor cells: Light-sensitive cells-rods and cones-on the retina that allow the eye to see in dim light, distinguish colors, and perceive contrast.
Piggyback intraocular lens: An IOL that is implanted on top of an existing IOL.
Pinhole acuity meter: Projection of an eye chart directly onto the retina, bypassing the lens, used to test potential acuity.
Posterior capsular opacification: Aftercataract; an opacity that can develop on the posterior capsule at any time after lens replacement.
Posterior capsule: The rear part of the lens capsule, which is left in place during cataract surgery to help support the implanted lens.
Posterior chamber: The fluid-filled area between the iris and the lens.
Posterior subcapsular cataract: A cataract that begins at the back of the lens, just under the lens capsule.
Potential acuity: A presurgical assessment of a patient's likely visual acuity if cataracts were removed.
Presbyopia: Loss of sharpness in near vision caused by age-related stiffening of the crystalline lens and accompanying reduction in ability to accommodate.
Pupil: Black circular opening in the center of the iris. Through muscular action of the iris, the pupil shrinks or grows (dilates) to regulate the amount of light that enters the eye.
Refraction: Bending of light as it passes from one material to another. Also, a test to determine the eye's refractive error.
Refractive error: Optical defect producing blurred vision due to light rays not converging precisely on the retina; nearsightedness, farsightedness, or astigmatism.
Refractive lens exchange: Like cataract surgery, a procedure to remove the crystalline lens and replace it with a synthetic lens. Refractive lens exchange, however, is performed before cataracts have developed significantly, generally because the patient cannot or does not wish to wear eyeglasses or contact lenses.
Refractive surgery: Procedure to correct refractive error, often by changing the shape of the cornea.
Retina: Smooth, thin layer of tissue, at the back of the eye, containing photoreceptor cells, which convert reflected light into electrical impulses that move along the optic nerve to the brain.
Retinal detachment: Separation of the retina from the underlying pigment epithelium, requiring immediate surgery to prevent blindness.
Retinal pigment epithelium: The part of the retina consisting of dark tissue cells that absorb excess light and carry nutrients to, and waste products from, the retina.
Ripe cataract: See mature cataract.
Rod: One of more than 120 million retinal photoreceptor cells (in each eye) that are especially receptive to brightness and allow us to see in dim light.
Sclera: The "white of the eye"; an opaque, fibrous, protective covering that surrounds the eye.
Second sight: A temporary, cataract-induced improvement in vision among nearsighted people.
Secondary cataract: See aftercataract.
Slit lamp: A microscope that projects a flattened beam of light into the eye for close examination of internal structures.
Snellen's chart: Standard assessment instrument for visual acuity; chart consisting of rows of letters (largest at the top, smallest at the bottom) developed by Dutch ophthalmologist Hermann Snellen in 1862; usually read at a distance of twenty feet.
Socket: The protective bony cavity that holds the eyeball.
Steroid: A drug, often a type of hormone, that is used medically to relieve swelling and inflammation.
Strabismus: Eye misalignment caused by imbalance in muscles that hold the eyeballs; often referred to as "cross-eye."
Subcapsular cataract: See posterior subcapsular cataract.
Tear: Thin film of fluid that lubricates the front of the eye. Blinking spreads tear film evenly across the surface.
Tonometer: An instrument, often used in glaucoma testing, that measures pressure of fluids inside the eye.
Tonometry: Measurement of intraocular pressure.
Toric intraocular lens: An IOL specially designed to correct astigmatism.
Traumatic cataract: A cataract that is caused by direct eye injury, head injury near the eye, earlier eye surgery, eye inflammation, chemical burns, or electric shock. Some scientists consider radiation a form of "slow trauma" that contributes to cataract development.
Tunic: One of three layers of the eyeball that surround the fluid-filled center.
Ultrasound: High-energy sound waves, often projected onto internal structures, creating echoes of different magnitudes that can be visualized on a television screen.
Ultrasound biometry: See A-scan.
Ultraviolet radiation (UV): Electromagnetic radiation, shorter in wavelength than visible radiation but longer than X-rays; invisible rays of the sun responsible for damage to skin and eyes.
Uvea, uveal tract: Eye layer between retina and sclera that contains the iris, ciliary body, and choroid.
Uveitis: Inflammation of the uvea.
Visual acuity: Sharpness of vision.
Visual field: Extent of the area visible to an eye looking straight ahead; includes central and peripheral vision.
Vitrectomy: Surgical removal of the vitreous, which is replaced with clear fluid.
Vitreous, vitreous humor: Clear gel-like substance that fills the rear two-thirds of the eyeball, between the lens and the retina.
Wall-eyes: See exotropia.
YAG laser: Yttrium aluminum garnet laser, which produces a short-pulse, high-energy light beam to cut or perforate tissue.
Zonule: One of the fibers that connect the ciliary muscle to the crystalline lens. Contraction and relaxation of the ciliary muscle change the tension of the fibers, which in turn changes the focusing power of the eye. The fibers also help to hold the lens in place.
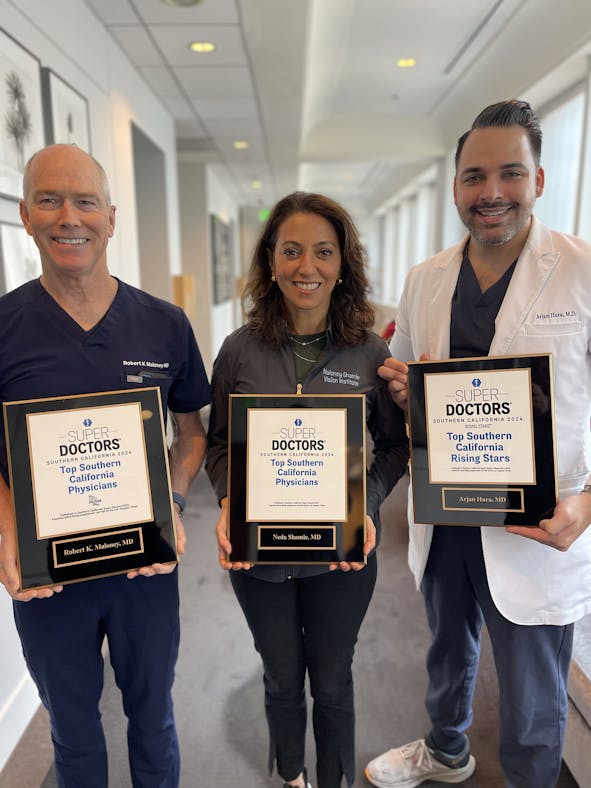
About Dr. Maloney